What is a Credit Balance?
A credit balance in medical billing occurs when a patient or insurance company pays more than the amount owed for healthcare services. This results in a negative balance on the patient's account and must be reviewed and resolved to maintain financial accuracy and regulatory compliance.
Step-by-Step Credit Balance Process
1. Credit Balance Identification
Credit balances are identified through:
Patient account audits
AR aging reports
Payment posting reviews
Monthly or quarterly financial reconciliations
Early identification helps prevent compliance risks and revenue inaccuracies.
2. Credit Balance Analysis
Once identified, each credit balance is reviewed to determine the root cause, such as:
Insurance overpayment
Duplicate payments
Incorrect charge entry
Contractual adjustment errors
Patient overpayments
Proper analysis ensures the correct resolution path.
3. Verification & Documentation
The billing team verifies:
Original charges
EOB/ERA details
Patient payment history
Insurance contracts
All findings are documented to support audits and payment communication.
4. Pay or Patient Resolution
Based on the analysis:
Insurance overpayments are refunded to the payer
Patient overpayments are refunded or applied to future balances (with patient consent)
Timely refunds are critical to meet compliance requirements.
5. Adjustment Posting
Correct financial adjustments are posted in the billing system to:
Clear the credit balance
Reflect accurate revenue
Maintain clean AR accounts
This step ensures correct accounting records.
6. Quality Check & Compliance Review
Before closure:
Accounts are reviewed for accuracy
Compliance guidelines are checked
Refund documentation is validated
This minimizes audit risks and errors.
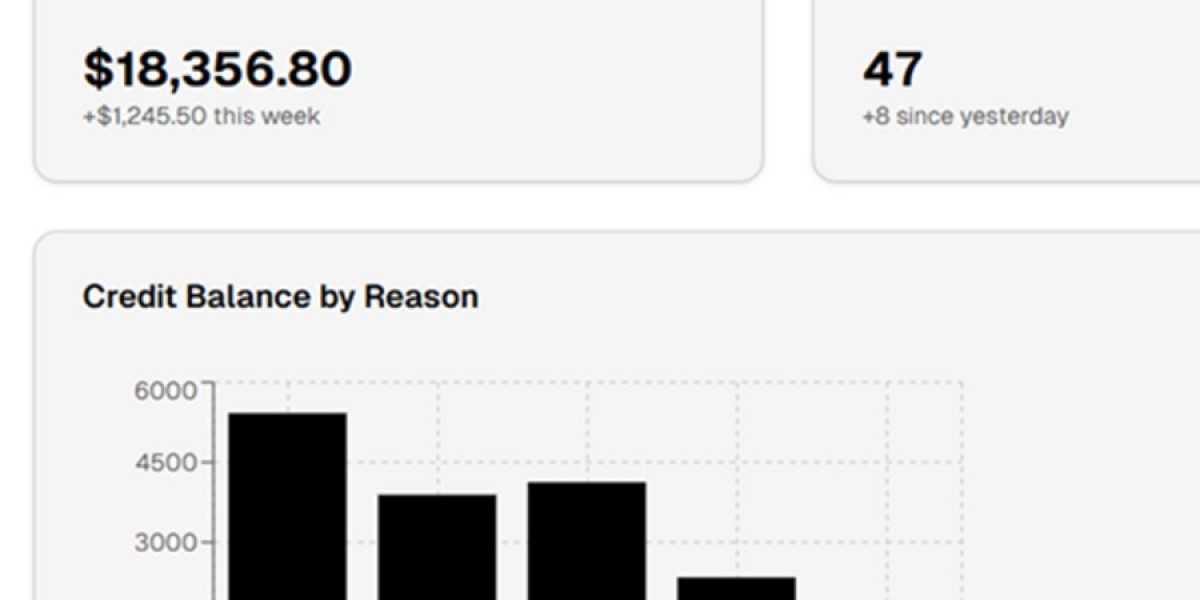
7. Reporting & Monitoring
Regular reporting includes:
Credit balance trends
Root cause analysis
Prevention strategies
Ongoing monitoring helps reduce future credit balance occurrences.
Why Credit Balance Management is Important
Prevents regulatory penalties
Maintains accurate financial records
Improves patient satisfaction
Improves overall revenue cycle efficiency
Conclusion
The credit balance process in medical billing is a vital component of revenue cycle management. A structured and compliant approach ensures accurate refunds, clean AR, and financial transparency. Proper credit balance handling protects both healthcare providers and patients while supporting long-term revenue integrity.